We like to present readers with helpful tips and reminders about how they can best care for their veins. Occasionally, it’s worth returning to the basics with a brief refresher about how the venous system works and some of the issues that may arise within it. Having knowledge about the development and symptoms of venous disease may enable you to recognize it in yourself, or a loved one, and start treatment sooner.
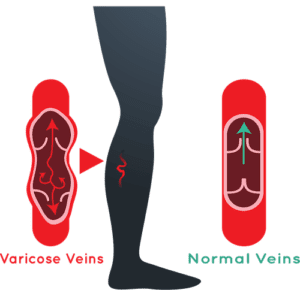
The venous system is the network of veins that return blood to the heart. This means that throughout much of the body veins are fighting against gravity as they move blood vertically. The mechanisms within veins that facilitate the upward movement of blood are special one-way valves that, when closed, look like an inverted ‘V’. As blood moves up, the valves open to let it through and then close to prevent the blood from flowing back down. In this way, the blood inches back up the veins to the heart. This process is fairly straightforward, and typically remains so as long as veins stay healthy. However, if the vein walls or valves are damaged, then problems are likely forthcoming. While vein issues can develop anywhere in the body, they are especially common in the legs and pelvis.
Most people are familiar with spider veins and varicose veins, and many can see one or both of these types of veins in their own legs. In some cases spider veins are purely cosmetic, but in other cases they, like varicose veins, indicate that the vein valves are malfunctioning by not closing tightly enough to seal and prevent the backflow of blood. The result is that blood pools in the veins, which can ultimately stretch the vein walls, create pressure throughout the system, and cause tiny red and blue networks of spider veins, or bulging, ropey varicose veins to appear.
This condition is referred to as chronic venous insufficiency or, more simply, venous disease. There is no single cause of this condition, and it can be difficult to pinpoint attributing factors. In some cases genetics plays a significant role, in others lifestyle. The contraction of muscles in the legs help pump blood through the veins, so people who sit or stand at work for sustained periods may be at greater risk. That said, athletes can also develop spider and varicose veins! Pregnancy is a risk factor for developing venous disease, and it may result from a plain old injury. A significant portion of the population is susceptible to venous disease, so if you develop it, you’re in good company and shouldn’t blame yourself.
Many of the symptoms of venous disease, other than the appearance of spider or varicose veins, can be felt. Chronic aching in the legs, itchiness around the ankles, feelings of pressure or fullness in the lower legs, swelling, skin discoloration, throbbing, cramping, or just nagging pain may all signal that there is a problem needing to be addressed. It can be easy to ignore these symptoms or misattribute them to other causes. If they don’t cease soon, however, it’s worth talking to a medical professional about them.
The progression of venous disease can be slowed or halted, but not reversed. Once the valves begin failing and causing problems, steps can be taken to mitigate the effects (for example, wearing compression stockings to create more pressure on leg tissues to facilitate blood flow) or a person may choose to undergo a treatment that can eliminate the problem fully. Seeking guidance on the best course of action is advisable, since modern technology enables vein specialists to determine the severity of the disease. Regardless of the approach that one ultimately chooses, it is important to deal with venous disease once diagnosed. Without appropriate intervention, venous disease can create more serious problems like blood clots and skin ulcerations.
Most modern treatment protocols and procedures are non or minimally invasive. In the mildest cases, a vein specialist might recommend that a patient wear compression stockings and regularly elevate the feet above the heart, and perhaps prescribe medications that assist with blood flow. If the case is more advanced, a patient will want to consider endovenous laser ablation or sclerotherapy. In rare but severe cases, surgery may be the best course of action. Fortunately, in any of these scenarios the patient will not experience much discomfort. Procedures such as laser ablation or sclerotherapy typically take place in outpatient vein clinics and only require a few hours per session. Most post-procedure discomfort is manageable with over-the-counter pain medications.
If you have heard friends or family members mention that they are experiencing some of the symptoms described in this article, it’s worth sharing your knowledge about venous disease and recommending that they get checked out by a vein specialist or personal physician. Your suggestion could result in saving them a lot of health trouble in the long run and easing pain that is diminishing their quality of life. At Artemis we are always glad to discuss over the phone a person’s symptoms, and suggest whether coming in for a consultation is a good idea. We are a highly experienced medical team backed by state-of-the-art technology, and we take great pride in providing excellent care. Give us a call today or visit us online and we will help put you on the path to better wellness.